Comprehensive Guide to Endometriosis Treatment in the UK
Exploring the Historical Development of Endometriosis Management

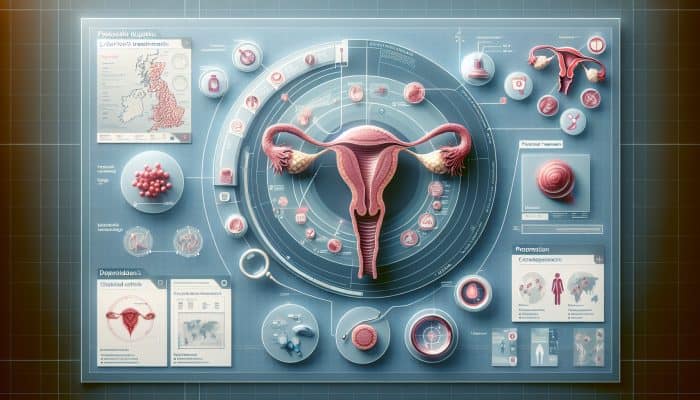
Endometriosis Treatment Trends: The treatment landscape for endometriosis in the UK has a complex history that mirrors broader advances in medical knowledge and practice. Historically, treatment approaches primarily focused on symptom relief rather than addressing the underlying causes of the condition. Many women endured lengthy and often frustrating diagnostic journeys, frequently facing substantial delays before accessing suitable care. Early treatment methods predominantly centred around pain relief, utilising analgesics and hormonal therapies without a comprehensive understanding of the disease itself. This limited approach often led to a frustrating cycle for many women, who sought relief but found that satisfactory results were not always achievable.
The late 20th century marked a significant shift in the management of endometriosis, driven by major advances in medical research. The advent of laparoscopic surgery revolutionised the diagnostic process, enabling healthcare professionals to accurately identify and treat the condition by removing endometrial tissue that had previously gone unchecked. This era marked the beginning of a more patient-focused approach, which emphasised considering individual cases and recognising the profound impact of endometriosis on women's lives.
In the UK, management of endometriosis continues to evolve, significantly influenced by ongoing research and the perspectives of those affected by this debilitating condition. The current focus lies on customising treatments to meet the unique needs of individuals, acknowledging the intricate and diverse nature of endometriosis and its effects on women's health.
Exploring the Current Standard Treatments for Endometriosis
Present-day treatments for endometriosis in the UK include a range of options tailored to the distinctive needs and circumstances of individual patients. The cornerstone of treatment typically includes hormonal therapies, which aim to manage symptoms by regulating or suppressing hormonal fluctuations that can exacerbate the condition. These therapies are frequently personalised, with choices ranging from oral contraceptives to progestins and GnRH agonists, each designed to alleviate the specific symptoms experienced by the patient.
In addition to hormonal treatments, effective pain management strategies are crucial to the overall treatment plan. Non-steroidal anti-inflammatory drugs (NSAIDs) are commonly prescribed to relieve pain, while alternative therapies like acupuncture and physiotherapy are increasingly recognised as valuable complementary approaches. These interventions not only aim to reduce pain but also strive to enhance the overall quality of life for individuals living with endometriosis.
For many individuals grappling with severe endometriosis, surgical interventions remain a vital treatment option. Laparoscopic surgery is routinely performed to excise endometrial implants and adhesions, with the preservation of reproductive capability often being a priority when fertility is a concern. In such cases, specialised surgical techniques are employed to optimise outcomes and enhance the chances of successful conception.
It is imperative for patients in the UK to engage in open discussions with their healthcare providers to explore available treatment options and collaboratively determine the most suitable course of action for their unique circumstances.
Uncovering Emerging Therapies and Ongoing Research in Endometriosis
Emerging therapies in the UK signal promising advances in the management of endometriosis, with ongoing research exploring innovative drug treatments and minimally invasive surgical techniques. One of the most exciting developments involves the introduction of novel medications targeting specific pathways implicated in the disease process. For example, research into aromatase inhibitors and new hormonal agents has the potential to improve symptom management while minimising side effects for patients.
Research institutions throughout the UK are actively investigating the genetic and molecular underpinnings of endometriosis to identify biomarkers that could facilitate earlier diagnosis and the development of personalised treatment strategies. Trials involving new combinations of drugs are underway, promising a more nuanced approach to addressing the symptoms of endometriosis. This emphasis on precision medicine is crucial, as it acknowledges the disease's unique manifestations across individuals and aims to deliver targeted therapies that align with those variations.
In surgical interventions, the advent of robotic-assisted laparoscopic surgery is enabling greater precision and shorter recovery times. These innovative techniques are poised to transform the treatment of endometriosis, enabling tailored surgical approaches that can lead to better outcomes and increased patient satisfaction.
As research progresses, the potential for breakthroughs in the management of endometriosis becomes increasingly tangible, fostering hope and optimism for those affected by this chronic condition.
Understanding Access to Endometriosis Treatment Across the UK

Access to endometriosis treatment in the UK varies significantly by location, healthcare policy, and resource availability. Although many regions have seen improvements in awareness and management of endometriosis, many patients still face substantial barriers to care. The National Health Service (NHS) aims to provide equitable access to treatment; however, the reality often diverges considerably across regions.
In urban centres, patients frequently benefit from access to specialised clinics devoted to endometriosis care. These facilities typically employ multidisciplinary teams, comprising gynaecologists, pain specialists, and mental health professionals, to deliver comprehensive care. Conversely, patients in rural areas may face delays in diagnosis and treatment due to a lack of specialised services and long referral wait times.
Moreover, regional healthcare policies can significantly influence the availability of specific treatments, particularly advanced therapies or surgical procedures. Patients may need to advocate for their needs and explore private healthcare options if local services do not adequately meet their needs.
Public awareness campaigns have begun to tackle these disparities, aiming to educate both healthcare professionals and the general public on the critical importance of timely diagnosis and treatment. Additionally, access to patient support groups and educational resources has expanded, empowering individuals to navigate treatment options more effectively and with greater confidence.
Enhancing Patient Support and Education on Endometriosis
Support groups and educational resources are vital to managing endometriosis in the UK, providing essential guidance and community support for those affected. These resources empower patients by fostering a sense of community and shared understanding, which can significantly alleviate feelings of isolation and frustration that often accompany endometriosis.
Local and national organisations play a critical role in disseminating information about the disease, available treatments, and effective coping strategies. These groups frequently organise workshops, seminars, and online forums, enabling individuals to connect with others facing similar challenges. Such peer support can be invaluable, offering emotional encouragement and practical advice on navigating the healthcare system and managing symptoms effectively.
Furthermore, education is essential to empowering patients. A thorough understanding of endometriosis, its symptoms, and treatment options enables individuals to take an active role in their care. Many healthcare providers in the UK now prioritise patient education as a fundamental component of treatment, ensuring patients are well informed about their condition and the options available to them.
In recent years, online platforms have significantly expanded access to information and support, enabling individuals to seek guidance from home. This shift has been particularly beneficial during periods of restricted in-person gatherings, highlighting the resilience and adaptability of the endometriosis community as they continue to support one another.
Insights from Experts on Current Trends in Endometriosis Treatment
Showcasing Real-World Examples of Successful Treatments

Real-world examples of successful endometriosis treatments in the UK demonstrate the diverse approaches used to manage this complex condition. Below are several notable case studies that illustrate positive patient outcomes:
- A patient who underwent laparoscopic excision surgery experienced a remarkable reduction in pain and an enhanced quality of life, allowing her to resume daily activities with renewed ease.
- A woman treated with a combination of hormonal therapies reported a remarkable 60% decrease in her symptoms and improved regularity of her menstrual cycle.
- A patient participated in a comprehensive pain management programme that included physiotherapy and acupuncture, successfully managing her symptoms without relying solely on medication.
- After participating in a clinical trial of a new medication, a patient reported sustained symptom relief and improved emotional well-being, underscoring the potential of novel therapeutic options.
These examples underscore the significance of personalised treatment plans, which can lead to improved patient satisfaction and superior outcomes.
Providing Actionable Steps for Healthcare Professionals
Healthcare professionals in the UK can stay informed about the latest advances in endometriosis treatment by implementing several practical strategies. Engaging in continuous medical education, attending specialised conferences, and participating in workshops can significantly enhance their expertise. Furthermore, collaborating with multidisciplinary teams ensures a holistic approach to patient care, thereby improving treatment outcomes and overall patient satisfaction.
Offering Expert Analysis on Future Trends in Endometriosis Treatment
The future of endometriosis treatment in the UK appears promising, with anticipated breakthroughs in personalised medicine and biologics. Progress in understanding the molecular basis of endometriosis may lead to the development of more targeted therapies, shifting treatment paradigms from generic approaches to tailored interventions that address each patient's unique needs.
Understanding the Role of Multidisciplinary Teams in Endometriosis Treatment
The integration of multidisciplinary teams is crucial for enhancing endometriosis treatment outcomes in the UK. By bringing together the expertise of gynaecologists, pain specialists, nutritionists, and mental health professionals, these teams can deliver comprehensive care that addresses all facets of the patient's experience. Collaborative care ensures treatment plans are holistic, considering both physical and emotional health, leading to improved patient outcomes and satisfaction.
Emphasising the Importance of Patient Education and Support
Educating patients about endometriosis is essential in the UK, as it empowers them to take charge of their health journey. A thorough understanding of the condition, its symptoms, and treatment options enables individuals to make informed decisions, enhancing treatment adherence and overall well-being. Moreover, access to robust support systems, including counselling and peer support groups, fosters resilience and assists patients in navigating the complexities of living with endometriosis.
How Have Endometriosis Treatments Evolved in the UK?
What were the early treatment methods for endometriosis?
The early treatments for endometriosis in the UK encompassed a variety of hormonal therapies and surgical options. Hormonal treatments aimed to manage symptoms, but often failed to address the fundamental disease process. Although surgical interventions were available, they were often invasive and did not consistently deliver effective results, resulting in variable patient outcomes and satisfaction.
What advancements have been made in recent years regarding endometriosis treatments?
Recent advancements in the UK have dramatically transformed the treatment landscape for endometriosis. Enhancements in laparoscopic surgical techniques have rendered procedures less invasive, resulting in shorter recovery times and fewer complications. Additionally, the emergence of targeted medications, such as newer hormonal therapies and anti-inflammatory drugs, aims to deliver more effective symptom relief and significantly improve patients' quality of life.
How have patient outcomes improved over time in endometriosis treatment?
Patient outcomes in the UK have improved markedly over time, largely due to advances in diagnostic tools and treatment options. With greater awareness and understanding of endometriosis, healthcare professionals are better equipped to provide timely, effective interventions. Consequently, many individuals enjoy an enhanced quality of life and greater satisfaction with their treatment journeys, reflecting the positive evolution of care practices.
Identifying Challenges in Endometriosis Treatment in the UK
What are the barriers to effective treatment for endometriosis?
Barriers to effective endometriosis treatment in the UK include limited awareness among healthcare providers, which often results in diagnostic delays. Many patients report long wait times for specialist appointments and limited access to multidisciplinary care. These challenges can lead to feelings of frustration and exacerbate symptoms, ultimately affecting patient outcomes and overall quality of care.
How do healthcare disparities affect access to endometriosis treatment?
Healthcare disparities significantly impact access to endometriosis treatment in the UK, with individuals in rural areas frequently facing longer wait times and fewer options compared to those in urban centres. The availability of specialised endometriosis clinics varies significantly, resulting in inequitable access to care and treatment. This disparity underscores the urgent need for targeted policies to address gaps in service provision.
What role does funding play in endometriosis research and treatment accessibility?
Funding is critical for advancing endometriosis research and ensuring treatment availability in the UK. Adequate financial resources facilitate the exploration of new therapies and the enhancement of healthcare services. Conversely, insufficient funding can hinder progress and limit the development of innovative treatments, ultimately affecting the quality of care patients receive.
How can policy changes improve endometriosis care in the UK?
Policy changes in the UK have the potential to significantly improve endometriosis care. By increasing research funding, reducing diagnostic delays, and enhancing access to specialised treatments, policymakers can improve patient outcomes. Implementing comprehensive guidelines for the management of endometriosis can also standardise care and ensure equitable access nationwide, benefiting all individuals affected by this condition.
Proven Strategies for Advancing Endometriosis Treatment Trends
Expert Recommendations for Comprehensive Patient Care
Expert recommendations for managing endometriosis in the UK underscore the importance of a holistic treatment approach. Combining medical interventions with lifestyle adjustments—such as dietary modifications, regular physical activity, and effective stress management—can significantly enhance symptom management and overall well-being for patients living with this condition.
Evidence-Based Treatment Options for Endometriosis
Evidence-based treatment options for endometriosis in the UK include a diverse range of hormonal and surgical interventions that have demonstrated effectiveness in clinical trials. These include the use of GnRH agonists and laparoscopic excision surgery, both of which offer significant benefits in terms of symptom reduction and improvements in patients' quality of life.
Guidance for Navigating the Healthcare System for Endometriosis Treatment
Navigating the UK healthcare system for endometriosis treatment can be challenging. Patients can follow these key steps to enhance their experience and outcomes:
- Consult a general practitioner (GP) to discuss symptoms and seek a referral to a specialist.
- Request information about local endometriosis clinics and available support services.
- Stay informed about treatment options by accessing reputable online resources and organisations.
- Document symptoms and treatment responses to effectively communicate with healthcare providers.
Looking Ahead: Future Directions for Endometriosis Treatment in the UK
What are the potential breakthroughs on the horizon for endometriosis treatment?
Potential breakthroughs for endometriosis treatment in the UK include advancements in personalised medicine and gene therapies. These innovations have the potential to revolutionise care by offering tailored treatment approaches that target each patient's unique biological characteristics, enabling more effective symptom management and improved overall outcomes.
How can patient advocacy shape future treatment trends for endometriosis?
Patient advocacy in the UK plays an essential role in influencing trends in endometriosis treatment. By raising awareness and advocating for increased research and improved healthcare policies, advocacy groups can affect funding decisions and drive positive changes in care. This grassroots movement ensures that the voices and experiences of those affected by endometriosis are considered in shaping future treatment strategies.
What role will technology play in the future of endometriosis treatments?
Technology is poised to impact future endometriosis treatments in the UK significantly. Innovations like telemedicine, which enhances access to specialist consultations, and artificial intelligence, which aids in diagnostics, will improve the overall management of the condition. These advancements can facilitate quicker diagnoses, more personalised care, and ultimately better patient outcomes, making the journey towards effective treatment more accessible.
How might multidisciplinary approaches enhance endometriosis care in the future?
Multidisciplinary approaches to endometriosis care in the UK have the potential to improve treatment outcomes significantly. By integrating the expertise of a wide range of specialists—including gynaecologists, pain management experts, and mental health professionals—patients benefit from comprehensive care that addresses the multifaceted nature of the disease. This collaborative model fosters improved communication and coordinated care plans, leading to enhanced patient experiences and satisfaction.
What funding strategies are necessary for advancing endometriosis research?
Increased support from both government and private funding sources in the UK is vital for advancing research into endometriosis. By prioritising financial resources for studies that investigate new treatments and deepen our understanding of the disease, we can enable the development of innovative therapies and improve patient outcomes. A strategic investment in research is essential to drive progress and ensure that individuals affected by endometriosis receive the highest quality of care.
Frequently Asked Questions About Endometriosis
What is endometriosis?
Endometriosis is a chronic condition characterised by the growth of tissue similar to the uterine lining outside the uterus, often resulting in significant pain and potential fertility issues.
What are the common symptoms associated with endometriosis?
Symptoms of endometriosis can include pelvic pain, heavy menstrual bleeding, pain during intercourse, and infertility, among others, affecting the overall well-being of those impacted by the condition.
How is endometriosis diagnosed?
Endometriosis is primarily diagnosed through pelvic examinations and imaging tests, with laparoscopic surgery frequently employed for a definitive diagnosis and potential treatment during the same procedure.
What treatment options are available for managing endometriosis?
Treatment options for endometriosis encompass hormonal therapies, pain management strategies, and surgical interventions aimed at excising endometrial tissue, all tailored to meet the individual needs of patients.
Can dietary changes influence endometriosis symptoms?
Some studies suggest that dietary modifications, such as reducing intake of inflammatory foods, may help manage endometriosis symptoms, although individual responses may vary significantly.
Is endometriosis hereditary?
Evidence indicates that endometriosis may have a hereditary component, as it can run in families, although the precise causes and mechanisms remain under investigation.
How does endometriosis impact fertility?
Endometriosis can affect fertility by causing scarring and adhesions that interfere with the reproductive organs. However, many women with endometriosis are still able to conceive successfully.
What role do support groups play in managing endometriosis?
Support groups provide essential emotional and practical support for individuals with endometriosis, enabling them to connect with others facing similar challenges and share valuable coping strategies.
Are there any promising new treatments for endometriosis in development?
Research is ongoing, with numerous promising developments in personalised medicine and novel drug therapies aimed at delivering more effective treatment options for individuals living with endometriosis.
How can I advocate for improved endometriosis care?
You can advocate for better endometriosis care by raising awareness, engaging with advocacy groups, and working with healthcare policymakers to expand services and increase funding for research and treatment.